New Study Suggests Potential Health Concerns
The use of psychedelics like psilocybin, LSD, ketamine, and MDMA is growing in Canada, but researchers are now exploring the potential long-term risks associated with these substances.
A recent study suggests that individuals who seek emergency medical care after using psychedelics may face a higher risk of death within five years compared to the general population.
Psychedelics fall under the category of hallucinogenic drugs, and their popularity has surged in both Canada and the U.S. In the United States, the percentage of people reporting hallucinogen use more than doubled between 2016 and 2021, rising from 3.8% to 8.9%.
In Canada, about 5.9% of people used a psychedelic in 2023, with the number climbing to 13.9% among those aged 20 to 24, according to Dr. Daniel Myran, a physician and researcher at the University of Ottawa.
Myran said that while many people turn to psychedelics for potential mental health benefits, clear evidence on long-term safety is still lacking. Clinical trials typically exclude individuals who may be at higher risk, so real-world data is needed to better understand the risks.
ER Visits and Hospitalizations Examined
To assess the connection between hallucinogen use and long-term health outcomes, researchers analyzed Ontario health data from over 11.4 million people aged 15 to 105. They focused on individuals who had been treated in emergency departments, hospitalized, or seen by physicians for issues related to psychedelic use.
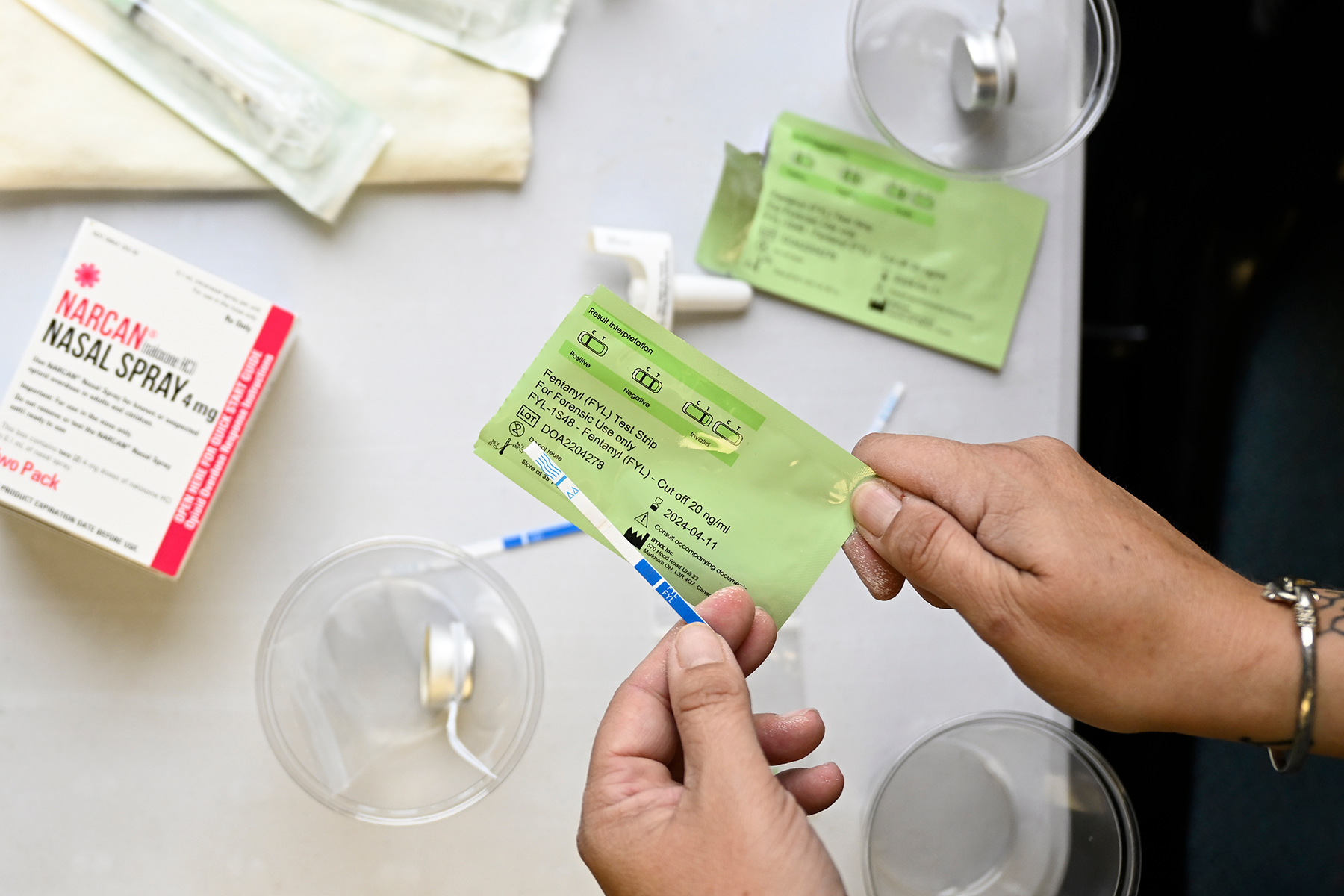
Among this group, 7,954 people sought emergency care after using hallucinogens, often due to severe anxiety attacks, distressing hallucinations, or other adverse reactions.
“This group is particularly vulnerable and needs close observation, intervention, and risk-reduction strategies,” Myran explained.
The study found that within five years, 6.1% (482 people) of those who had required medical attention for hallucinogen use had died, compared to just 0.6% (460 people) in the general population of the same age and sex.
However, Myran cautioned that the study does not establish psychedelics as the cause of these deaths. When researchers examined the causes of death, they found higher rates of suicide, drug poisoning, lung disease, and cancer, which may indicate other underlying health issues or lifestyle factors, such as increased smoking rates.
“Seeing an increase in suicide raises concerns about whether psychedelics play a role,” Myran noted.
Limitations and Calls for Further Research
The study had some limitations—it did not specify which hallucinogens were used or how they were consumed. Additionally, those who ended up in emergency care for psychedelic use were more likely to have pre-existing health conditions, including asthma, high blood pressure, depression, and substance use disorders.
Given the rising popularity of psychedelics outside of clinical settings, the study’s authors emphasize the need for continued research on both potential risks and benefits.
Medical Experts Weigh In
Dr. Jennifer Swainson, a psychiatrist at Edmonton’s Misericordia Community Hospital and an expert on ketamine treatment for depression, says that while the risks shouldn’t be ignored, they should also be kept in perspective.
She compared the 7,000 hallucinogen-related hospital visits in the study to the nearly 400,000 hospitalizations linked to alcohol and more than 70,000 for opioids and stimulants like methamphetamine.
Swainson stressed that medical supervision is crucial when using psychedelics, particularly for individuals with a personal or family history of mental illness or substance use issues.
“These substances impact the brain, and their effects vary depending on a person’s underlying mental health,” she explained. “Used improperly, they carry risks—but that doesn’t mean they should be over-vilified.”